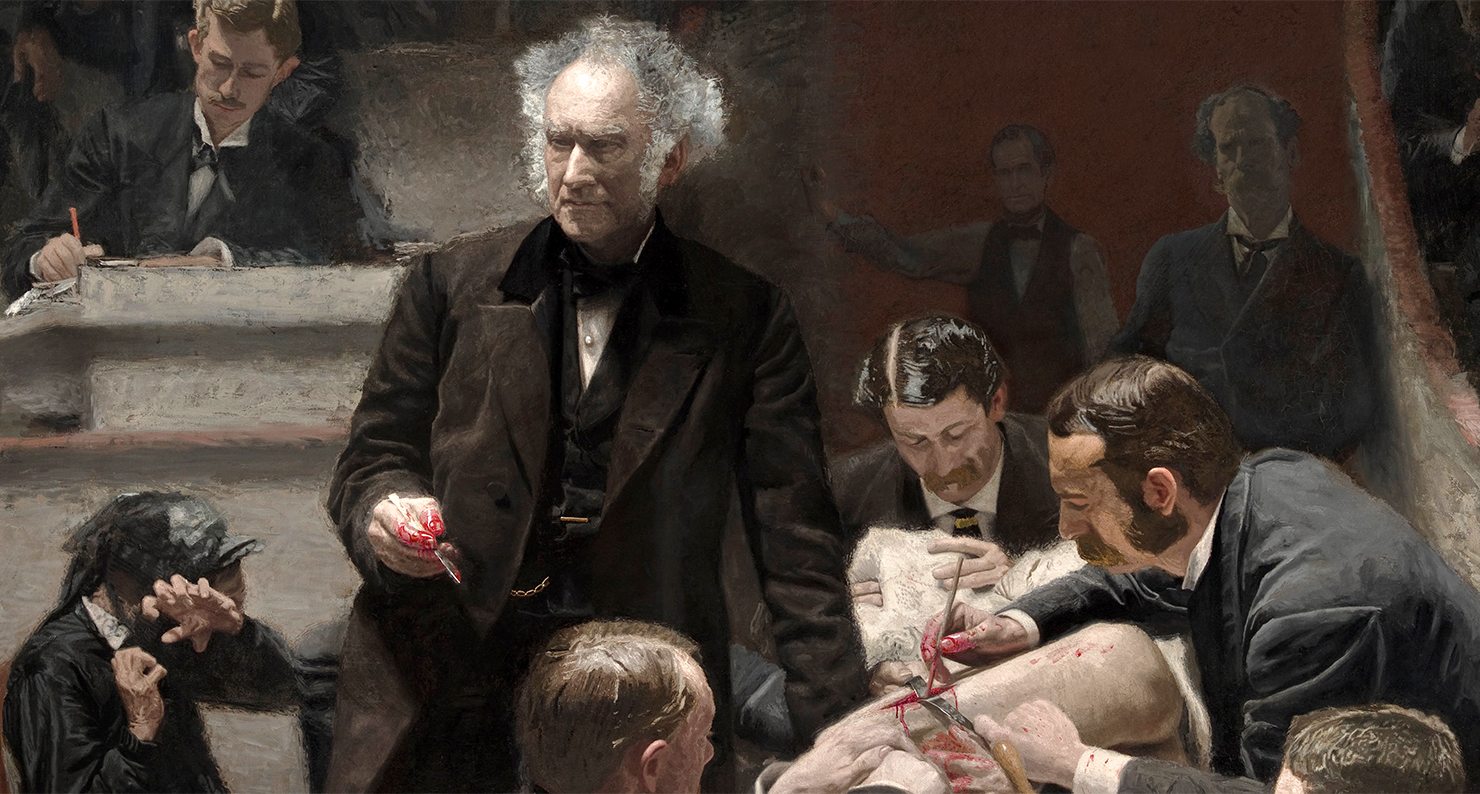
Portrait of Dr. Samuel D. Gross (The Gross Clinic), by Thomas Eakins, 1875. Philadelphia Museum of Art, Gift of the Alumni Association to Jefferson Medical College in 1878 and purchased by the Pennsylvania Academy of the Fine Arts and the Philadelphia Museum of Art in 2007.
By the time I began my emergency medicine rotation, I had come a long way from making that first tremulous incision into a cadaver during anatomy class. Back then, at the beginning of first year, I remember trying to conceal my apprehension as we removed an opaque plastic sheet from the supine body.
We had all prepared for this moment, as a class and in our own ways, but still my heart raced as we uncovered first the feet, then the legs, then the torso, like an outgoing tide slowly revealing hidden details of a beach or rocky shore. Once the sheet was fully lifted from the body, the face remained shrouded by a damp cloth. We would get into that later in the course.
Less than three years later, I had been around a fair amount of death. I had seen children born without brains on pediatrics, known people who died in code-blues on the internal medicine floors, and seen others bleed out on the operating table during surgery.
In the emergency department we got a bit of everything, and one night a call came in from an approaching ambulance carrying a teen-aged female in cardiac arrest. They didn’t tell us anything more, and in the eerie minutes before the ambulance arrived doctors and nurses took their places and we got one of the trauma bays ready with IVs, medications, and intubation equipment. There was a respiratory technician student there as well, and we both positioned ourselves behind our respective instructors, close enough to be available if called upon, but far enough to be out of the way.
A few awkward moments passed once everything was ready. One nurse asked the emergency medicine resident about his weekend. Another repositioned the medication cart. Then the patient was brought in: obese, sweatpants and sports bra, pale lips, IV line dangling from the antecubital vein inside her right elbow. We moved her from the stretcher onto the trauma bed as one of the paramedics handed over a bag of saline with one hand while continuing chest compressions with the other. His partner recounted the ride, telling us little more than that the patient had been found pulseless and had remained so despite continued CPR.
We cut off the rest of the girl’s clothes while one of the nurses slid a second IV into her left AC and another took over compressions, pausing briefly to allow the resident to work the blade of the laryngoscope down the patient’s throat, slip a breathing tube just beyond the vocal cords, and inflate a small balloon to hold it in place as compressions and ventilation resumed.
Every couple of minutes the activity paused and we all looked at the monitor for a “shockable” rhythm, something to indicate electrical activity. Each time, the pulse disappeared, blood pressure tanked, and the line on the monitor flattened out. Glances in the direction of the attending physician running the show became more frequent.
“Have you gotten to do compressions yet?” someone asked the other student.
“No” she replied, and was promptly positioned on a stool for better leverage.
Having been assigned to the seemingly more menial ventilation bag, I felt a twinge of envy. Then surprise, recalling how recently just being in the hospital had filled me with excitement. Then guilt, as I turned my attention back to the girl lying on the bed, riddled with tubes and needles.
“You let us know if you get tired,” one of the nurses told the respiratory student.
“I’m fine,” she replied quickly.
“Ah, the eagerness of youth,” someone said, “enjoy it while it lasts.”
Everybody chuckled.
“The family is here,” relayed a nurse from the hallway.
“Bring them in,” said the attending. A shaken but resolute man in his 70s walked in first and came straight to the bedside to hold his granddaughter’s hand, tangled in IV lines and defibrillator leads.
She was dead. We all knew that. Her heart hadn’t beaten on its own for an hour. Chest compressions had kept some blood moving, but she had only gotten paler and cooler since she arrived, more and more like one of the cadavers from years before. But when her grandfather appeared, she was alive again. Well, not quite alive, and not quite again. Rather it was the first moment that I saw her as someone who had once been alive; who still was alive, in a sense, through her grandfather, and her tearful parents, and her silent siblings, and even her little niece, a wide-eyed girl in a gymnastics outfit clutching an unopened can of Pepsi.
As I looked around the room, it seemed obvious that death wasn’t about the dead. It was about the old man who by then had seen it all, and the parents whose lives would never be the same. It was about the little girl with the warm soda in her hand taking it all in, the scene and emotions already forming a memory that will be woven and unwoven for the rest of her life.
The mind is a real place. Thoughts and memories not only guide our actions, but they can change the pace of our heart, the rate of our breathing, even the size of our pupils. That we live on in the thoughts of others may offer little consolation in the face of one’s own death, but what could be more important than the half-hidden tracks we leave upon the minds of those close to us, and the marks they leave, in turn, on us.
It is little wonder that preoccupation with mortality and existential angst go hand in hand with underlying feelings of disconnectedness and isolation. Little wonder one of the most terrifying things about death for the famously withdrawn Philip Larkin is “nothing to love or link with.” Little wonder baby monkeys choose the cloth-covered figure over the wire one with food. Or, at least, little wonder we are moved by that gesture.
When the family showed up that night, everything and nothing changed. The only difference in management was moving the patient to a room in the ICU so resuscitation efforts could be withdrawn in private, with everyone together. Only the attending actually spoke to the parents, and it could not have been more than a few minutes from when the grandfather first arrived to when the patient was moved upstairs. Then, once they all left the trauma room, the sheets were changed, an intoxicated man with a scalp laceration was wheeled in, and I never saw any of them again.